Controlling pain after knee replacement surgery is critical to a quick recovery. If you fail at this point expect a much longer rehabilitation period.
STEP #1 Take your pain meds as directed
Expect large amounts of “chemically” induced pain-the kind your body normally secretes in response to “trauma,” the first two weeks.
Trying to bend your knee with pain levels greater than 5/10 is like banging your head against a wall…you simply won’t do it… or you’ll do it very infrequently until the pain lessens.
This is a huge waste of down time. A large majority of my patients are able to recover 110 to 120 degrees range of motion post-surgically in the initial two week period. Any veteran of knee replacement surgery, will tell you that getting the knee to bend fully is arguably one of the most difficult tasks after surgery.
This is why you should use your narcotic pain pills to their fullest advantage.
In most cases, you can be off the narcotics in two weeks. Once range of motion has been restored, building strength into the knee is a piece of cake by comparison and narcotics are overkill. [If you want more information on how to do this please consult my book.]
STEP #2 Take your pain meds as directed…if you can get them
Unfortunately today’s strategies for controlling pain after knee replacement are being overtaken by political crusaders against opioid addiction. Trust me, I get it: opioid addiction is real.
However, I just happen to be old enough to remember the misguided home health emphasis undertaken by the Centers for Medicare Services (CMS). They determined that no one suffer with “unmanageable” pain. We were to investigate pain levels every visit.
Most older patients instinctively knew that suffering with pain was better and more healthy than getting hooked on narcotics. However, persistent “sanctioning” can eventually dull the most sensible among us.

Narcotics started flying off the shelves like candy on Valentine’s Day, spawning a whole new industry of pain management specialists, a direct result of this official destigmatization.
Of course we have an opioid addiction problem, the medical establishment helped create it. But I digress…
In some states, you will now have to run the gauntlet like a convicted felon to get a narcotics supply that covers you for the initial two weeks. The best thing to do is to talk to your surgeon to find out his exact method for controlling pain after knee replacement.
Then find out how to deftly navigate the logistics of getting the help you need to succeed and thrive, not just survive this period.
State by state prescribing guidelines and whether they have the force of law behind them (your physician is mandated to follow them), can be found here.
STEP #3 Identify Whether You Fit The Likely Profile Of Someone Who Has Trouble Stopping Narcotics After Surgery
Whose NOT at risk?
If you have never used opioid medications prior to surgery, you have a less than .65 % chance of getting hooked long term.
Who is MOST at risk?
Patients who use opioids intensively prior to surgery for at least 4 months are most at risk.

In a recent study, 72% of persistent preoperative users were still using opioids one year after knee replacement surgery.
Presence of chronic pain-related co-morbidities like back pain or fibromyalgia were also associated with long term opioid use.
A general profile of someone likely to have trouble tapering off narcotics after knee replacement surgery consists of:
- female sex
- older than 50 years
- preoperative history of drug abuse, alcohol abuse, depression, benzodiazepine use, or antidepressant use.
Benzodiazepines are anti-anxiety drugs sold under names like Clonazepam, Diazepam, Xanax and Lorazepam.
Opioids happen to be a very good choice for pain control if you are “opioid-naive.” They are effective and generally well tolerated for short periods to help you maximize your knee replacement recovery.
The effectiveness of opioids diminishes with significant preoperative use and they place you at greater risk of prolonged hospital stays, complications and early revision surgery.
So make a commitment to taper off opioids prior to surgery if at all possible! You’ll be glad you did; good things will follow in the wake.
Alarming Trends in Knee Replacement Pain Control?
As I mentioned above, we are in the midst of a profound change in prescribing habits for knee replacement pain control.
During research for this article, I ran across an interesting report entitled, “Exposing a Silent Gateway To Persistent Opioid Use.”
The report promoted three key “alarmist” findings.
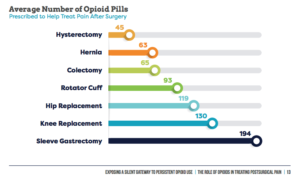
1. Opioids to treat post-surgical pain continue to be overprescribed
2. High potency opioids pose risks for orthopedic surgery patients
3. Surgery leads to long-term use of opioids, putting patients at risk of addiction and dependence
While there is some truth in these findings, I labeled them “alarmist” because I think they overexaggerate the true risk that opioids pose.
The most vulnerable surgical candidates represent a narrow minority with a closely defined profile. They could be counseled prior to surgery and perhaps given a different course of treatment. This is a classic case of throwing the baby out with the bathwater because a certain segment is vulnerable.
So who is behind this publication? Let’s connect the dots.
The Opioid Epidemic and Knee Replacement Surgery
The report, “Exposing a Silent Gateway To Persistent Opioid Use.” is found on the website, www.planagainstpain.com
The authors state that their mission is to examine national and state-by-state opioid prescribing trends and the the role that opioid-based post-surgical pain management plays in contributing to the nation’s opioid drug crisis.
The Centers for Disease Control and Prevention (CDC) has declared that we have an opioid epidemic in the United States. Overdoses involving heroin, fentanyl and prescription opioids killed more than 33,000 people in the United States in 2015. Nearly half of those deaths were from prescription opioids.
Following along with this line of thinking approximately 15,000 deaths result from those abusing prescription drugs.
However, I found no attempt, in the report, to separate “deaths from legally obtained prescription drugs” and “deaths from illegally obtained prescription drugs,” which to me is a fairly important distinction.
Hysterically, the report claims that, “Unused Opioids Threaten Families and Communities” and that “9 in 10 surgery patients with leftover opioid pills admit that they haven’t properly disposed of them.”
If this is true, then let’s find a way to educate surgical patients in proper disposal instead of controlling access to everyone and limiting the actual benefits of pain meds based on the actions of the few.
Just Who Is A Persistent or Long-Term Narcotic User?
In addition the report claims that 15.2% of knee replacement patients went on to long-term use of opioids. A closer look reveals that “long term” user includes anyone still using at 3 – 6 months after the surgical procedure, which is not that uncommon especially when pain meds are used sparingly to start. Usually those people are still stuggling to get their range of motion back.
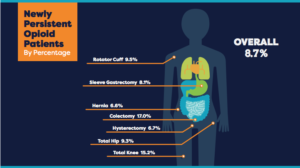
The number from less biased research concludes that 7% end up using “long term.” Their definition of “long term” being one year not 3-6 months. The majority of “long term” users fit the general profile that was previously outlined.
The authors recommended guidelines for opioid prescribing…
“if opioids are indicated for acute pain, initiate therapy at the lowest effective dose for no longer than a 3-5 day duration; reassess if pain persists beyond the anticipated duration.”
Marketing Masquerading as Research
Investigating more deeply and one finds…
The report was based on research from IQVIA Institute for Human Data Science and Wakefield Research with funding from Pacira Pharmaceuticals, Inc.
Pacira pharmaceuticals, coincidentally, is dedicated to “improving patient outcomes with opioid-reducing strategies”. Could this be because they market 3 classes of drugs for controlling pain after knee replacement that are in direct competition with opioid use? Hmm…
These drugs are
1. EXPAREL® (bupivacaine liposome injectable suspension) is a local analgesic administered at the time of surgery to control pain and reduce or eliminate the use of opioids for acute post-surgical pain.
2. The iovera system is a handheld cryoanalgesia device used to deliver precise, controlled doses of cold temperature only to targeted nerves, interrupting the nerve’s ability to transmit a pain signal.
3. DepoFoam® encapsulates drugs, preserving their molecular structure, and releases them over a desired period of time.
The copyright for the website, PlanAgainstPain shows Pacira’s ownership. Copyright @2019 Pacira BioSciences, Inc. Parsippany, NJ 07054
You can imagine the dismay of executives when three recent studies indicated that Exparel or liposomal bupivacaine wasn’t any more effective than the current standard of care in controlling pain after knee replacement surgery and it costs a lot more; driving up costs of care for everyone.
This report, funded by Pacira, in essence exaggerates opioid risk to sell more of their own product Exparel, which claims to reduce opioid dependence.
Summary: How to control pain after knee replacement
-
- Take your pain meds as directed.
- Figure out how to deftly navigate state/federal regulations so that you don’t waste time in recovery.
- Identify if you fit the profile of someone who might have trouble getting off narcotics and take action before surgery.
Resources
Kim SC, Choudhry N, Franklin JM, et al. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthritis Cartilage 2017 Sep;25(9):1399-406. DOI: https://doi.org/10.1016/j.joca.2017.04.002.
Lepasio MJ, Guarino AJ, Mont MA. Pain management associated with total joint arthroplasty: A primer. Perm J 2019;,23:18-169. DOI:http://doi.org.7812/18-169.

4 replies to "3 Easy Steps To Controlling Pain After Knee Replacement Surgery"
“Stoping” vs stopping
“Maquerading” vs masquerading
And many more. Article is full of spelling errors. You need a better proof reader
Thanks Ellen, rushed to get that one out and was very sloppy, will do better. Thanks again
I am now four months out of knee replacement. The nurses told me to do therapy, the DOC said “You don’t need therapy, just move!”
So everyday I moved. But now, when I try to BEND my knee and really push it, I come home in pain and worse than before. Am I doing too much?
It seems the harder I try, the stiffer I get. Doc is no help.
Is this normal? Should I just walk around and do my daily stuff and not push it?
Ok so the advice to “just move” everyday is terrible!!! You have to actually bend the knee to get back the range lost during the surgery. The earlier you do this the better off you are. Since you are now 4 months post op, you may need a manuipulation under anesthesia (MUA) to restore the range in your knee. I suggest you get my book follow the instructions for range of motion recovery for 2 weeks. If you can’t get the range to start improving– (you’ll know because you are measuring it), then follow up with a different MD and request a reevaluation of your situation.